Subscribe to our newsletter
Disclaimer: This article is for informational purposes only and does not constitute medical or legal advice. No HHS endorsement is implied.
Interoperability as the Universal Tech Translator
Let’s cut to the chase. Interoperability refers to the ability of different health IT systems to access, exchange, integrate, and utilize data in a coordinated manner. Think of it as the universal translator for your hospital’s technology. Getting it right isn’t just a tech project; it’s a business imperative that drives your most significant board-level metrics. It reduces waste from duplicate tests, cuts down on denied claims, and is now a regulatory necessity under the 21st Century Cures Act. For a typical 350-bed hospital; mastering interoperability can unlock over $1 million in annual savings from just one area: redundant lab work. This isn’t about chasing HIMSS stages. It’s about building a safer, more efficient, and financially sound organization. This is your roadmap.
Stop Chasing Milestones. Start Driving Metrics.
Look, we’ve sat in your chair. The board gives you a mandate—”Hit HIMSS EMRAM Stage 7 in 24 months”—and you’re stuck translating a technical journey into a language they understand: dollars and sense. Meanwhile, your clinicians are muttering about “change fatigue,” and your CFO hears “AI” and sees a money pit.
Let’s reframe the conversation. The real question isn’t: what is interoperability in healthcare? It’s “What business problems does it solve?“
Forget the jargon for a moment. Interoperability is about getting the right data to the right person at the right time. When it fails, the consequences are brutally tangible:
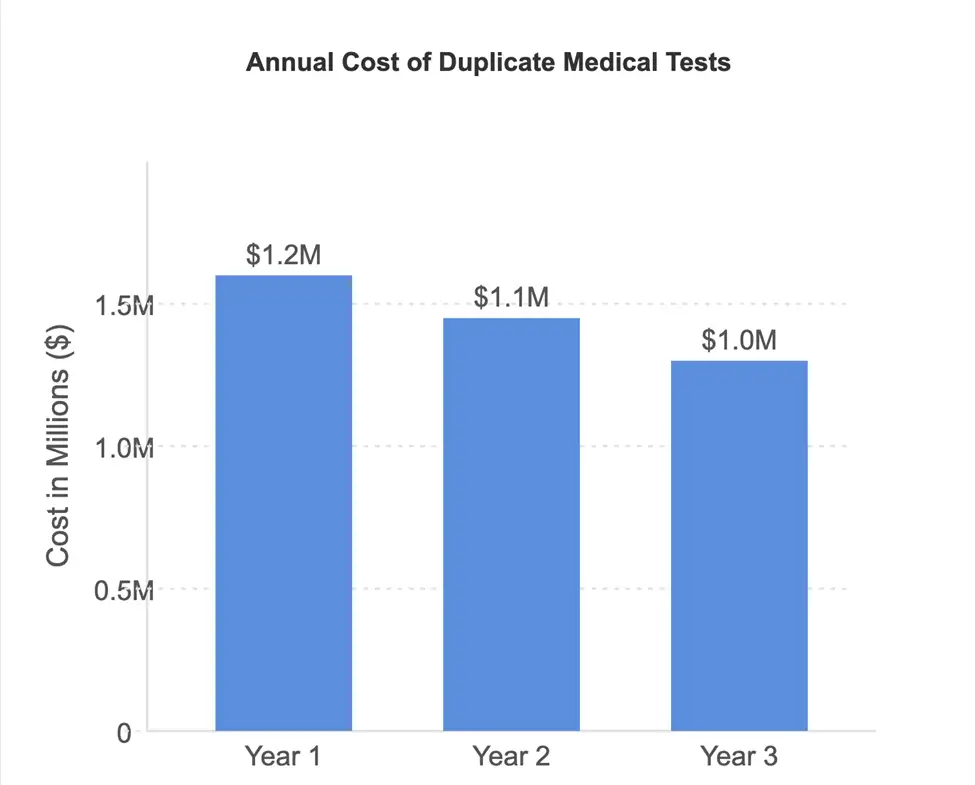
- The $1 Million Question: Your ED physician re-orders a CT scan because she can’t access the one from the clinic across the street. That’s not just poor patient care; it’s a direct hit to your bottom line. Studies have estimated that duplicate testing waste costs over $1 million annually for a 300-bed hospital.
- The Denied Claim Nightmare: A payer rejects a claim because the clinical documentation from the specialist’s EHR didn’t properly attach to the hospital’s billing file. That’s a revenue cycle headache born from a data silo.
- The Regulatory Hammer: Under the 21st Century Cures Act, if you knowingly interfere with the access, exchange, or use of electronic health information, you’re not just failing your patients—you’re “information blocking.” And as of mid-2024, that comes with real teeth, including significant penalties under programs like MIPS and the loss of eligibility for shared savings.
So, when the board asks about the ROI of your interoperability project, don’t show them a Gantt chart of interface engine upgrades. Show them a bar chart of declining duplicate test costs. Show them a trend line of reduced claim denials.
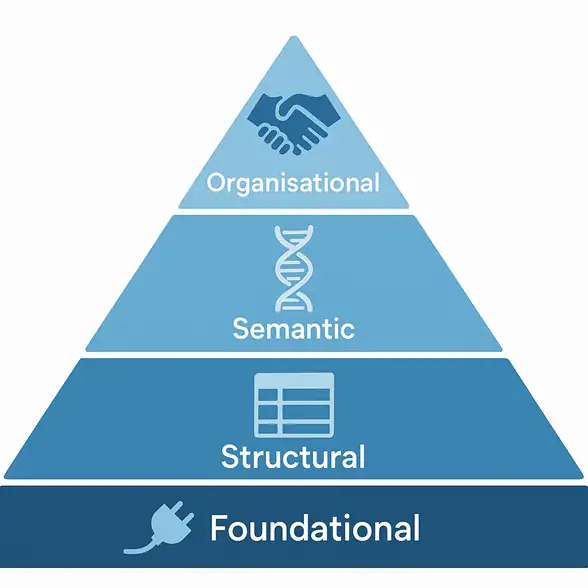
This isn’t about appeasing the tech gods. It’s about hard-nosed business strategy. Let’s break it down into the four layers, as defined by HIMSS, so you can build your plan.
Layer 1: Foundational Interoperability — The Digital Handshake
Let’s start with the basics. Foundational interoperability is digital plumbing. It ensures that one system can securely send a packet of data and another system can receive it. It doesn’t care what’s in the packet—it could be a PDF, an image, or a lab result. The receiving system can’t do much with the data other than store it and let a human read it. It’s the equivalent of faxing a record but without the paper jams.
And yes, in 2025, many organizations are still struggling with this.
- Regulation Tie-In: The 21st Century Cures Act’s most basic requirements hinge on this layer. Can you send a patient their record electronically upon request? If a patient uses an app to retrieve their data, your system must be able to respond accordingly. Failure is not an option and is considered a form of information blocking.
- Quick Self-Audit:
- Patient Record Request: Ask your HIM department: What’s our average turnaround time for a digital copy of a patient’s full record? If the answer is measured in days or involves manual steps, such as burning a CD, you have a foundational problem.
- Referral Packet: Ask a Care Coordinator: When we discharge a patient to an SNF, how does the record get there? If the answer is “we print and fax,” you’re looking at a foundational gap that’s leaking time and money and creating risk.
War Story: The “CD and a Prayer” Method
When I was CIO at a large health system, we acquired a string of physician practices. We discovered their “interoperability” with the local hospital was a courier who drove a batch of CDs with imaging files across town every evening. On Tuesday, the courier’s car broke down. An entire day’s worth of pre-op images for the next day’s surgeries didn’t make it. Chaos. We had surgeons and patients on-site, but no images were available. It was a stark, embarrassing lesson that foundational exchange isn’t just a convenience; it’s a critical infrastructure for patient safety. We fast-tracked a simple point-to-point VPN tunnel the very next week. It wasn’t elegant, but it was better than relying on a 1998 Toyota Corolla.
Layer 2: Structural Interoperability — Creating a Common Language
So your systems can exchange data packets. Great. However, we now need to ensure they can understand the structure of that data. Structural interoperability defines the syntax of the data exchange. It’s the difference between receiving a flat PDF (foundational) and receiving a structured message where your EHR can identify field A as “Patient Name,” field B as “Allergy,” and field C as “Medication.”
This is the world of standards like HL7® (Health Level Seven) and, increasingly, FHIR® (Fast Healthcare Interoperability Resources). It ensures that data is organized uniformly, allowing the receiving system to interpret it.
- Regulation Tie-In: The ONC’s Certification Program requires EHRs to be capable of consuming structured data using specific standards, such as the USCDI (United States Core Data for Interoperability). This is the technical underpinning of the Cures Act’s push for seamless data exchange. If your systems can’t process a standard CCDA (Consolidated Clinical Document Architecture), you’re falling behind.
- Quick Self-Audit:
- Medication Reconciliation: Sit with a nurse during an admission. When they pull in data from another hospital, does the medication list populate automatically into the right fields in your EHR, or are they manually re-typing it from a scanned document? That manual re-entry is the hallmark of a structural gap.
- Interface Inventory: Request a list of all your interfaces from your integration team. How many are using modern, API-based standards (like FHIR) versus older, clunky flat-file (FTP) transfers? This ratio is a direct indicator of your technical debt.
Vignette: The Allergy That Wasn’t
A 350-bed hospital in Ohio took pride in its new HIE connection. When a patient from a rival system was admitted to their ED, they successfully pulled his record. Foundational win! But the systems weren’t structurally aligned. The incoming data string for “Allergies” was formatted in a way their Cerner® system couldn’t parse. It appeared as a garbled note, not a discrete data field. The busy ED doc missed it. The patient, who had a severe penicillin allergy, was administered a penicillin-derivative antibiotic. The result was a preventable anaphylactic shock, a frantic ICU transfer, and a near-miss that became a system-wide call to action. They had exchanged the data, but they hadn’t used it. That failure in structural interoperability nearly cost a life.
Layer 3: Semantic Interoperability — Ensuring We Mean the Same Thing
This is the holy grail and, frankly, where the real magic happens. Semantic interoperability ensures that both the sending and receiving systems share a common understanding of the data’s meaning. It’s not enough to know that a field represents a lab result (structural); you need to know which specific lab result it is using a common vocabulary.
This is where coding systems like LOINC for labs, RxNorm for medications, and SNOMED CT for clinical terms become non-negotiable. It ensures that “systolic blood pressure” from an Epic® system means the same thing in a Meditech® system. Without this, data is ambiguous and dangerous.
- Regulation Tie-In: This is central to achieving high-value care and is implicitly required for advanced use cases, such as population health analytics and clinical quality reporting under MIPS. You can’t accurately report on diabetic patient outcomes if one system codes “HbA1c” one way and another codes it differently.
- Quick Self-Audit:
- Problem Lists: Pull problem lists for the same patient from two different connected systems (e.g., your inpatient EHR and an affiliated ambulatory clinic’s EHR). Are “Type 2 Diabetes” and “Diabetes Mellitus, Type II” treated as the same concept, or do they create duplicate entries?
- Quality Reporting: Ask your quality team how much manual data abstraction is required to submit their eCQMs (electronic Clinical Quality Measures). A high manual workload is a red flag for poor semantic alignment.
Mini Case Study: The Readmission Reduction Pilot
A Midwest health system ran a 12-month pilot connecting its flagship hospital’s Epic EHR with a large cardiology group’s Cerner system. Their goal was simple: reduce 30-day readmissions for congestive heart failure. By achieving true semantic interoperability for just three concepts—daily weight, diuretic dosage, and blood pressure—they created a shared dashboard that provided a unified view of patient data. The cardiologists could view the inpatient data in real-time, and the hospital discharge planners could track the ambulatory follow-up. They could act on a 2-pound weight gain before it became a full-blown crisis. The result? An 8% reduction in CHF readmissions in the first year, saving an illustrative $800,000 and, more importantly, keeping dozens of patients safe at home.
Layer 4: Organisational Interoperability — The Rules of the Road
You can have the best pipes, structure, and codebooks in the world, but if the people and policies don’t support data sharing, it’s all for naught. Organizational interoperability encompasses the governance, policies, legal agreements, and social frameworks that enable data sharing across entity boundaries.
But let’s be blunt. This is about trust. It’s about getting competing hospitals, insurers, and public health agencies to agree on the rules of engagement. It involves creating data-sharing agreements, establishing trust frameworks such as TEFCA, and ensuring that robust security protocols (including encryption, role-based access control, and audit logs) are in place to comply with HIPAA, GDPR, and other relevant privacy laws.
- Regulation Tie-In: This is the primary objective of TEFCA (the Trusted Exchange Framework and Common Agreement). It aims to establish a single “on-ramp” for nationwide health information exchange, governed by a common set of policies and technical requirements. Participation isn’t just a good idea; it’s becoming the standard for playing in the national sandbox.
- Quick Self-Audit:
- Data Governance: Do you have a formal data governance committee with charter and executive sponsorship? Who on that committee is empowered to make decisions about sharing data with an external partner? If you don’t know, you have an organizational gap.
- Onboarding a Partner: How long does it take, from initial request to live data feed, to connect a new community partner? If legal and administrative reviews dominate the timeline, your organizational layer is the bottleneck.
From the Field: The Governance Gauntlet
I once co-piloted what we called an “interface factory.” Our goal was to rapidly connect community physicians. The tech was easy—we could build an HL7 feed in our sleep. The bottleneck was what we referred to as the “Governance Gauntlet.” Every single connection required six signatures: our CIO, their practice manager, our legal counsel, their legal counsel, our security officer, and theirs. It took 90 days on average. We finally broke the logjam by creating a standardized, pre-approved “data sharing starter kit” with a lightweight agreement for common use cases. We traded some customizability for speed, which reduced our onboarding time by 75%. Sometimes, the best innovation isn’t a new technology but a simpler form.
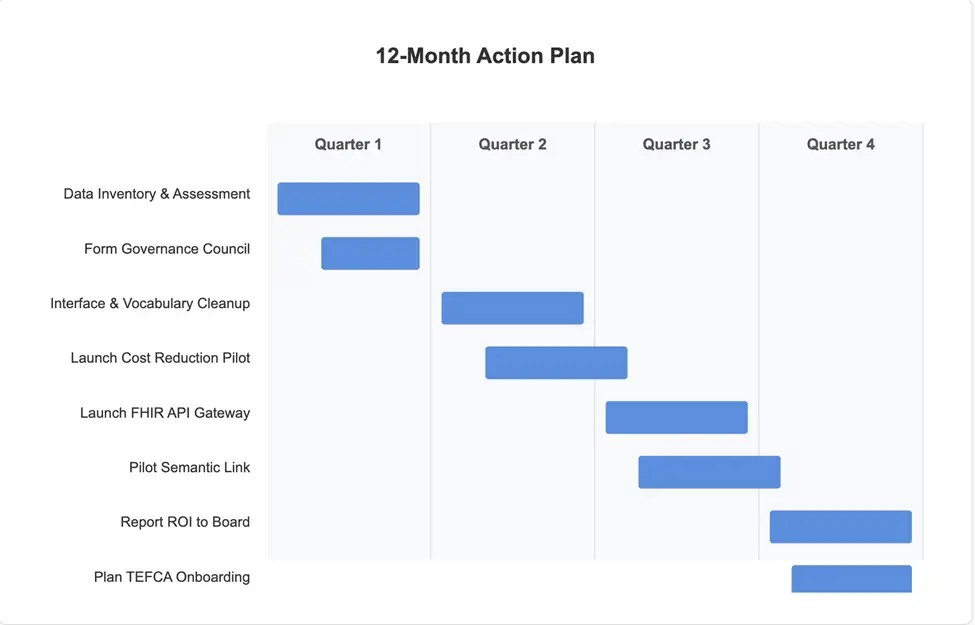
Your 12-Month Executive Action Plan
Look, this is a multi-year journey, but you can deliver tangible value within one fiscal year. Your board needs to see momentum and early wins.
Here is a simplified plan. Focus on cleaning up your own house first, then build bridges.
The Board-Ready ROI Table
This is an illustrative model for a 350-bed hospital. Plug in your numbers. The key is to frame the investment in terms of hard, operational savings.
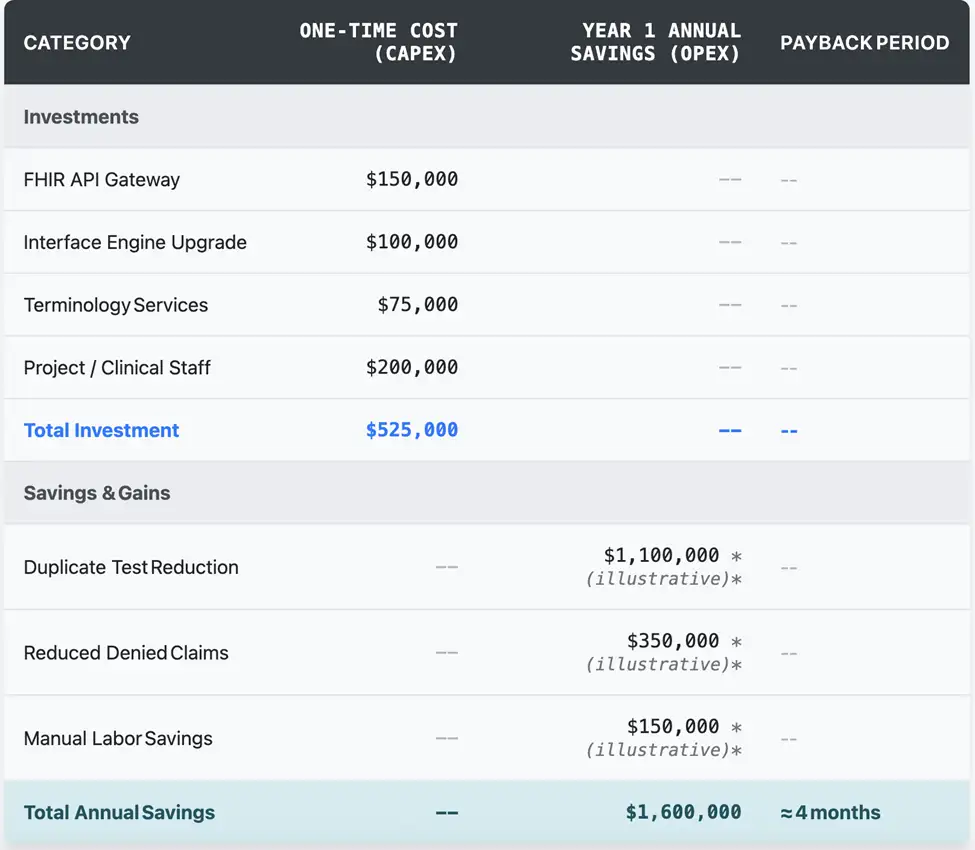
Note: All financial figures are illustrative and should be validated with your internal data.
Answering the Board’s Questions (Before They Ask)
You know they’re coming. Be ready.
1. What is interoperability, and is it a mandated requirement?
“Interoperability is how our different computer systems talk to each other. And yes, through the 21st Century Cures Act, federal rules now mandate that we share data electronically and can penalize us for ‘information blocking.’ This is a compliance issue as much as a technology one.”
2. This sounds expensive. What’s the real financial impact?
“There’s an upfront investment, but the return is significant and fast. We’re currently wasting over $1 million a year on duplicate tests alone because our systems can’t share data effectively. This project pays for itself by tackling that waste, reducing claim denials, and making our staff more efficient. The cost of inaction is far greater than the cost of investment.”
3. Our clinicians are already burned out. Is this just another thing for them to learn?
“This is designed to reduce their burden. True interoperability means less time hunting for records, fewer manual keystrokes re-entering data, and having a complete patient picture right in their workflow. When done right; this should feel like the technology is finally starting to work for them, not the other way around.”
The journey to full, seamless interoperability is a marathon, not a sprint. But it’s a race you have to run. By framing it in the language of ROI, risk mitigation, and regulatory compliance, you can turn your board’s skepticism into strategic alignment.
Ready to get started?
Let’s build your roadmap. Book a complimentary 30-minute white-boarding session with Logicon.