Subscribe to our newsletter
If you’ve ever faced a boardroom skeptical about digital transformation in healthcare, you’re not alone. Metrics speak louder than milestones. HIMSS Stage 7 validation isn’t just a plaque on the wall; it’s proof your hospital’s digital investments yield clinical quality, financial return, and better patient outcomes. But achieving Stage 7 within two years isn’t easy. How do you get there? We distill the journey into five core metrics: CPOE utilization, medication administration accuracy, structured documentation, barcode specimen tracking, and predictive analytics for sepsis. This roadmap provides quarterly checkpoints, realistic financial ROI, and a touch of humor—because healthcare transformation needs it.
Metrics Over Milestones: Why Boards Prefer Numbers
Look, no one loves another dashboard—but boards crave clarity. When CFOs and CEOs hear “digital transformation,” they think, “Show me the numbers.” Milestones might be impressive to IT teams, but board members think in terms of measurable outcomes. From my days leading digital change at Texas Health Resources, I recall our CFO’s candid call: “Ed, if you want buy-in, start speaking in dollar signs and decimal points.” Metrics not only quantify progress but also justify financial investments. Quantified outcomes, such as reduced medication errors, improved clinician documentation, and decreased sepsis mortality, compel boards to invest and clinicians to embrace change.
Metric 1: CPOE Utilization ≥ 90% for ≥ 4 Months
Lay Definition: Computerized Physician Order Entry (CPOE) refers to the process by which doctors enter treatment orders electronically, thereby reducing manual errors.
Stage 7 Requirement: HIMSS mandates sustained usage of≥ 90% CPOE for validation.¹
Two-Step Self-Audit:
- Check your current CPOE usage rate: Is it consistently over 85%?
- Evaluate physician training: Can clinicians articulate the value of CPOE beyond “management wants it”?
When I led the THR rollout, achieving our 90% target felt like Groundhog Day. We’d one cardiologist who would famously quip, “Computers are for Facebook, not medicine!” But after showing him our medication error reduction—from dozens per month down to fewer than three—he became our most prominent advocate. And yes, he now follows me on LinkedIn.
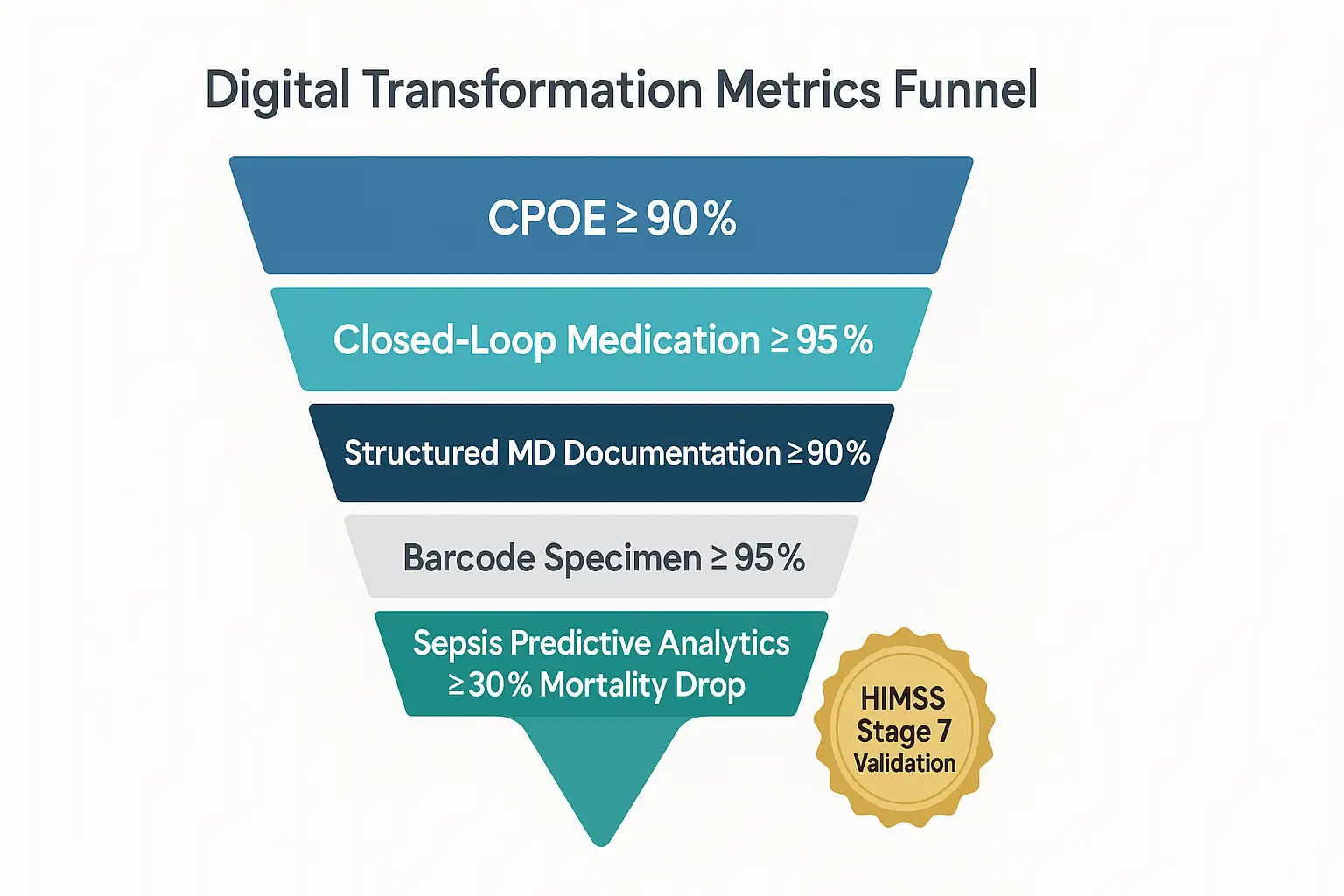
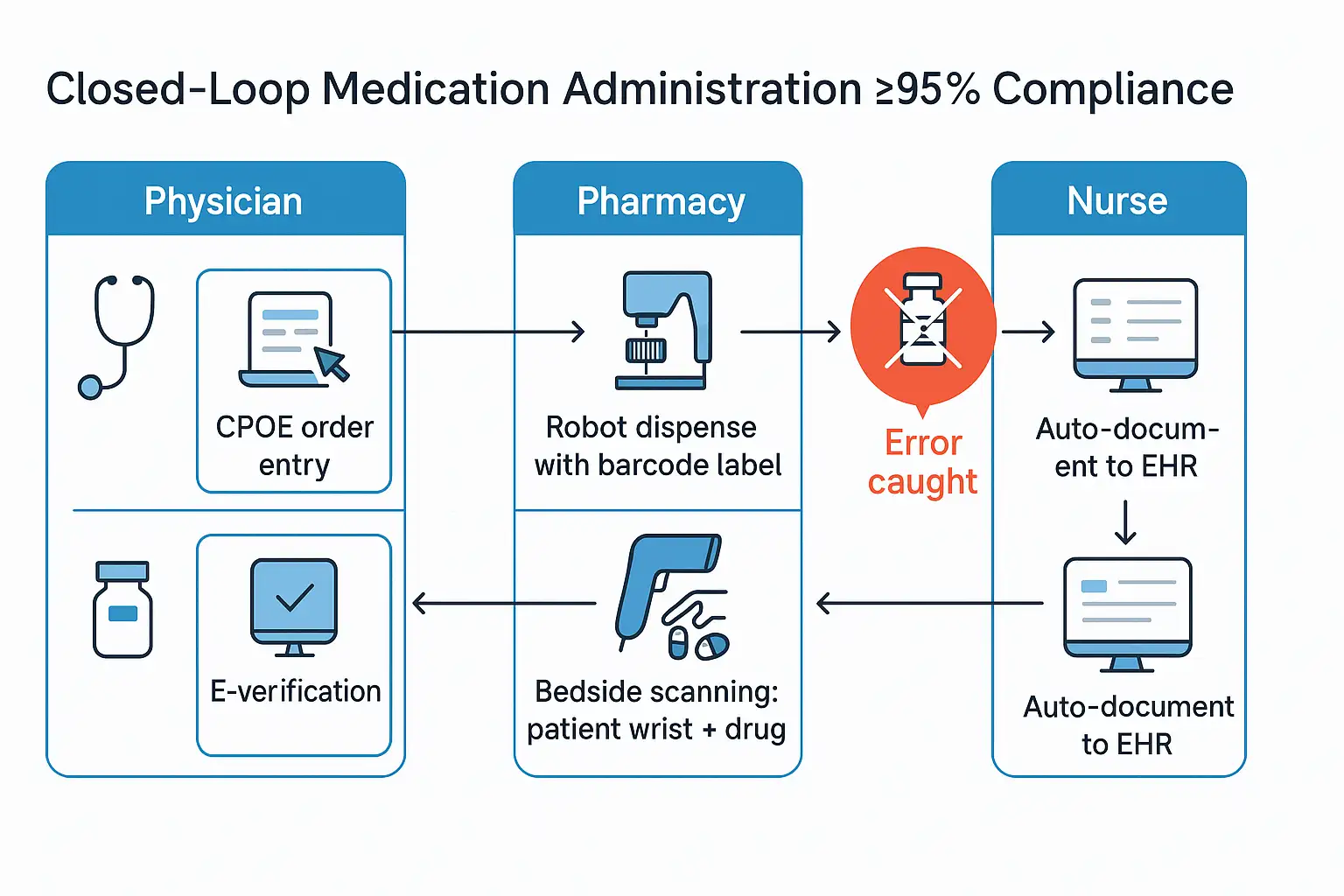
Metric 2: Closed-Loop Medication Administration ≥ 95%
Lay Definition: Ensures medications are correctly ordered, dispensed, administered, and documented electronically to minimize medication errors.
Stage 7 Requirement: Closed-loop medication processes must reach ≥ 95% compliance.²
Two-Step Self-Audit:
- Assess medication error rates: Are manual errors still creeping in?
- Review nurse workflows: Can nurses easily scan meds bedside without workarounds?
At one Midwestern hospital, we found that nurses were bypassing barcode scans to save time, which led to preventable errors. After streamlining workflows and retraining, we hit 97% compliance. The nurses even hosted a “barcode party” (yes, a cake shaped like a barcode). Humor aside, closed-loop medication saves lives and budgets.
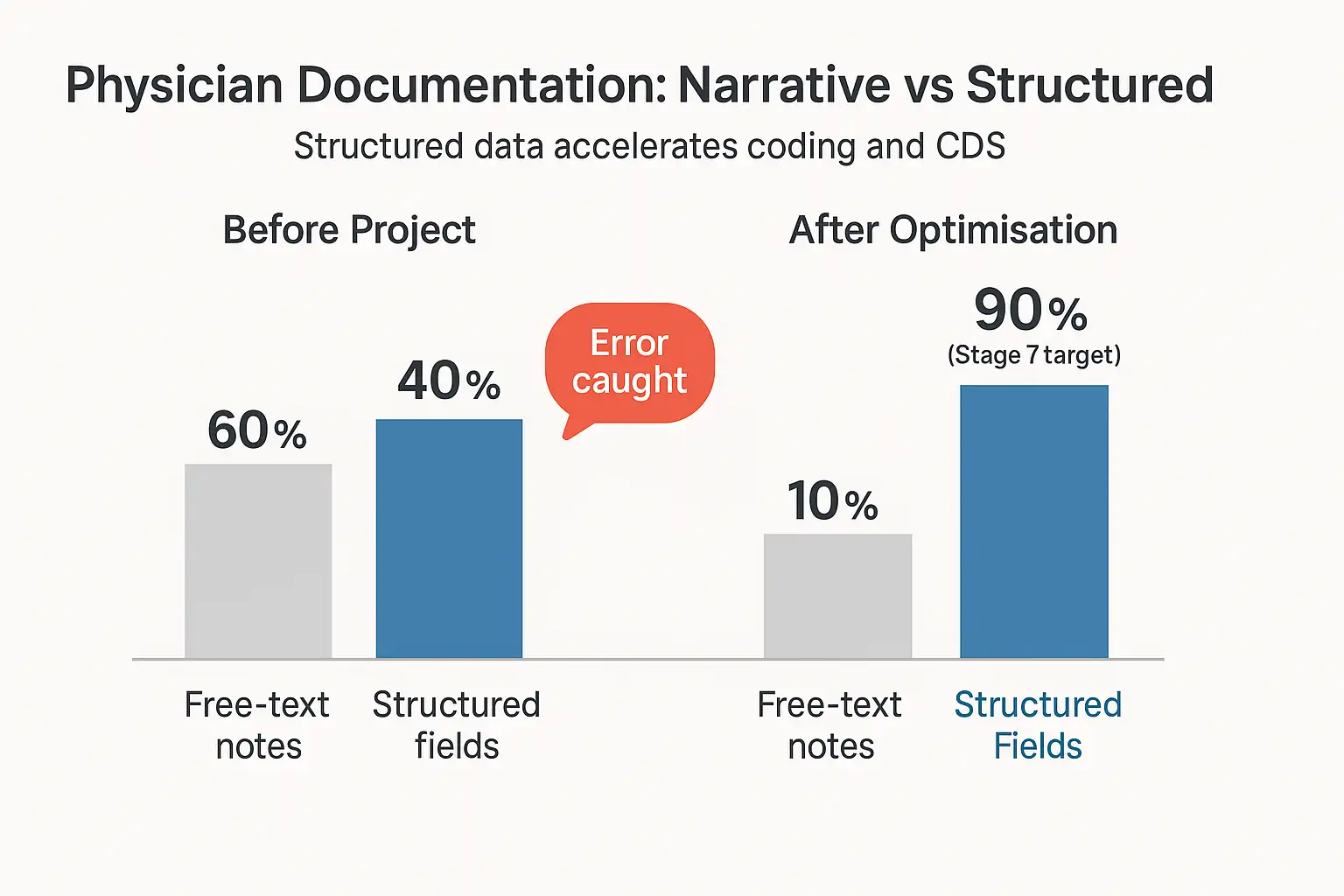
Metric 3: Structured Physician Documentation ≥ 90% Discrete Data
Lay Definition: Physicians document patient notes electronically in discrete, analyzable fields rather than free-text narratives.
Stage 7 Requirement: HIMSS requires ≥ 90% structured, discrete physician documentation.³
Two-Step Self-Audit:
- Audit current documentation: Are doctors still favoring narrative notes?
- Ease-of-use evaluation: Is EHR documentation intuitive and user-friendly?
We once found a surgeon dictating notes to a tape recorder—yes, an actual cassette—in 2020! Shifting him to structured documentation wasn’t an overnight process, but discrete data led to faster coding, more accurate billing, and fewer denials. Revenue cycle management improved significantly, and our surgeon reluctantly admitted, “Okay, digital’s faster than tape.”
Metric 4: Specimen/Blood-Product Barcode Scanning ≥ 95%
Lay Definition: Specimens and blood products must be barcoded and scanned electronically to prevent errors in patient identification.
Stage 7 Requirement: Barcode scanning compliance must exceed ≥ 95%, aligning with Joint Commission sentinel-event alerts.⁴
Two-Step Self-Audit:
- Analyze specimen error rates: How frequently are samples misidentified?
- Assess barcode workflow: Is barcode scanning seamlessly integrated into clinical practice?
A colleague at a 300-bed hospital once called this “the metric nobody loves until it saves a patient.” And that’s precisely what happened when our barcode system prevented a potentially fatal mismatch during a transfusion. Clinicians quickly became barcode evangelists—even sporting “Scan or Bust” stickers.
[Insert barcode scanning compliance graph]
Metric 5: Predictive Analytics Metric ≥ 30% Sepsis Mortality Drop
Lay Definition: Using AI-driven analytics to predict sepsis earlier, reducing mortality rates.
Stage 7 Requirement: Demonstrate analytics-driven sepsis mortality reduction ≥ 30%, inspired by Duke Health’s Sepsis Watch.⁵
Two-Step Self-Audit:
- Review sepsis mortality data: Do you have a clear baseline mortality measurement?
- Evaluate analytic readiness: Is predictive analytics operational in clinical workflows?
At Cleveland Clinic, implementing predictive sepsis analytics initially drew skepticism. One doc joked, “AI—Another Irritation?” But after seeing a 35% mortality drop within a year, skeptics became champions. Clinicians trusted data-driven alerts, and the board saw measurable ROI.
[Insert predictive analytics impact graph]
Your 24-Month Roadmap to HIMSS Stage 7
Here’s your quarter-by-quarter plan to hit Stage 7:
| Quarter | Milestones |
| Q1–Q2 | Baseline audits, infrastructure investment, clinician training |
| Q3–Q4 | Achieve CPOE ≥ 90%, Closed-loop med admin ≥ 80% |
| Q5–Q6 | Structured documentation ≥ 75%, barcode scanning ≥ 90% |
| Q7 | Predictive analytics pilot, refine workflows |
| Q8 | All metrics at Stage 7 levels, final audit prep |
ROI Snapshot (24-month projection)
| Metric | CapEx ($) | Annual Savings ($) | Payback Period |
| CPOE | 150k | 250k (error reduction) | 8 months |
| Closed-loop Med | 200k | 400k (med errors) | 6 months |
| Structured Doc | 100k | 350k (coding/billing) | 4 months |
| Barcode Scanning | 120k | 200k (specimen errors) | 7 months |
| Predictive Analytics | 300k | 600k (mortality reduction, LOS) | 6 months |
Mini-FAQs: Digital Transformation in Healthcare
Why prioritize metrics over milestones?
Metrics quantify progress and justify investment clearly to boards.
Is predictive analytics worth it?
Yes—proven ROI includes significant clinical improvements, such as Duke’s sepsis mortality drop.
What’s the most significant barrier to reaching Stage 7?
Clinician buy-in. Address with clear benefit communication and workflow optimization.
Ready to Transform?
Metrics drive clarity, clinician buy-in, and measurable ROI. Let’s map your path to Stage 7.
Book a 30-minute whiteboard session with Logicon.