Subscribe to our newsletter
The pressure on hospital operations has never been greater. Faced with persistent staff shortages, razor-thin operating margins, and overwhelming administrative burdens, healthcare leaders are turning to a powerful new ally: artificial intelligence. While the term “AI” can seem abstract, its practical application—Intelligent Automation—delivers tangible results. For operations directors, this means smoother patient flow, optimized supply chains, and a less-burdened workforce. For the CIO, it means a secure, integrated, and data-driven enterprise. This guide cuts through the hype to focus on five high-impact workflows where AI is already delivering a significant return on investment, from patient progression and documentation to staffing and revenue cycle management. By strategically deploying automation, health systems can build a more resilient, efficient, and sustainable operational core.
The Market Momentum & The Mandate for Change
The question is no longer if health systems should adopt AI, but how and how quickly. The data paints a clear picture of a sector at a tipping point. Margins are hovering at a precarious average of just 2.5%, leaving no room for operational inefficiency. This financial strain is compounded by a historic labor crisis, with nurse vacancy rates climbing to 18% and physicians spending nearly 4.5 hours per day on documentation and administrative tasks.
The market is responding to this pressure with urgency. The healthcare AI market is already valued at over $8 billion, and a recent survey revealed that 56% of hospitals now have a formal AI strategy in place. This isn’t innovation for innovation’s sake; it’s a necessary response to fundamental economic and workforce challenges.
For hospital executives, the mandate is clear: find ways to do more with less, without compromising care quality or burning out staff. Intelligent automation is the most potent tool available to meet this mandate, creating capacity, reducing friction, and freeing clinicians to focus on patients, not paperwork.
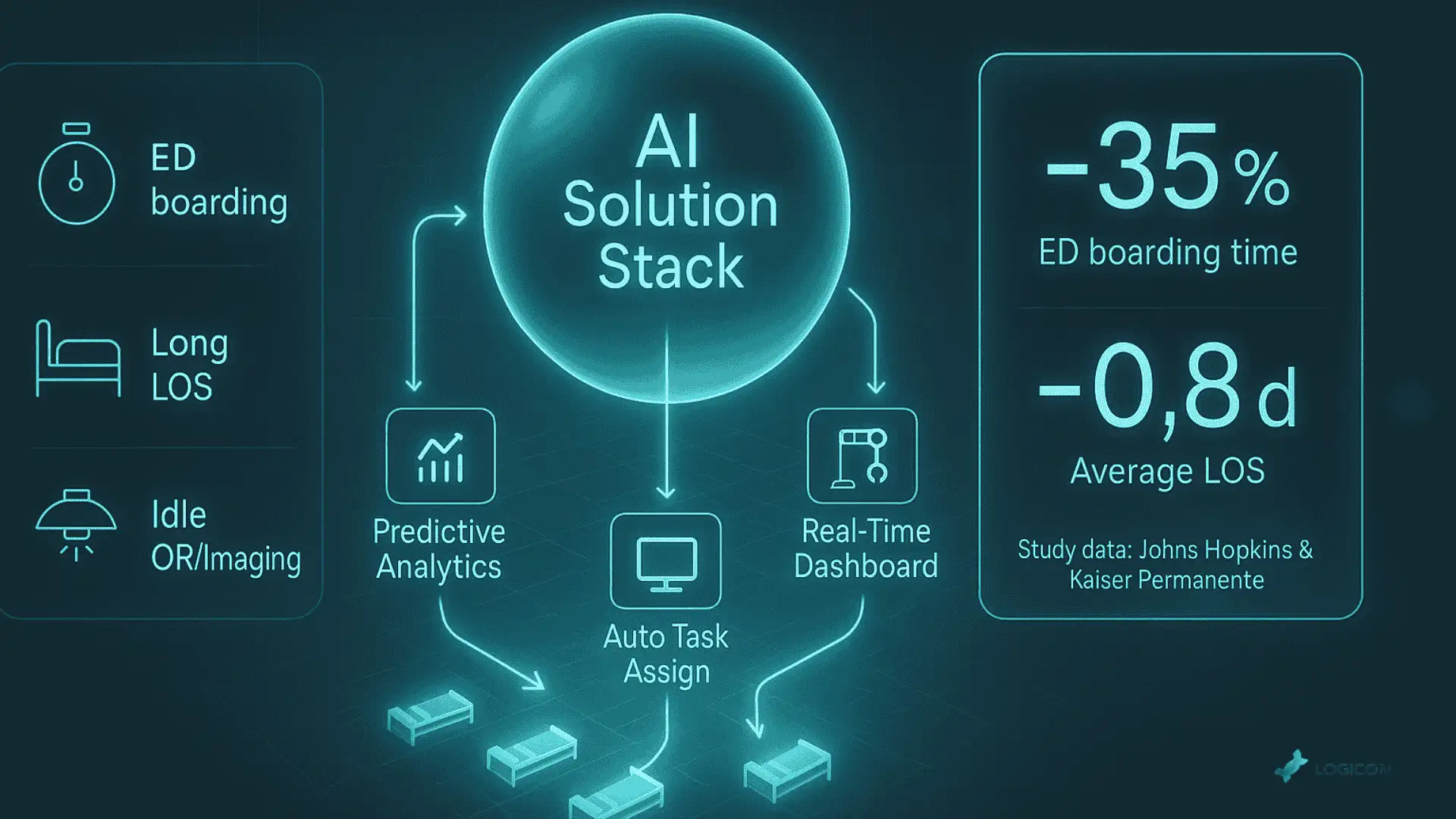
Workflow 1: Patient Flow & Capacity Management
Gridlock in the emergency department, long wait times for inpatient beds, and delayed discharges are more than just operational headaches—they directly impact patient safety and the bottom line. AI-powered command centers are turning this chaotic process into a predictable, manageable system.
The Pain Points
- Excessive Emergency Department (ED) boarding times.
- Lengthy patient stays (LOS) are driven by discharge bottlenecks.
- Underutilization of operating rooms and diagnostic suites due to poor scheduling.
The AI Solution Set
- Predictive Analytics: AI models analyze historical data from Admission, Discharge, Transfer (ADT) systems to forecast patient census, predict admission surges, and anticipate discharge-ready patients hours in advance.
- Real-Time Dashboards: A central command center visualizes bed availability, patient status, and staffing levels across the entire hospital, using AI to flag potential bottlenecks before they occur.
- Automated Task Assignment: The system can automatically assign transport and environmental services requests as soon as a discharge order is entered, significantly reducing bed turnover time.
Implementation Essentials
Success hinges on seamless integration between the AI platform and the core EHR, ADT, and ancillary department systems. Change management is critical for bed managers and charge nurses, shifting their role from reactive problem-solving to proactive, data-driven decision-making.
KPI & ROI Snapshot
- Primary Metrics: Average Length of Stay (LOS), ED boarding hours, bed turnover time, patient satisfaction scores.
- Average ROI: One notable study at Johns Hopkins showed a 35% reduction in ED boarding times, while Kaiser Permanente has used similar tools to decrease LOS by an average of 0.8 days.
Mini-Case Vignette
A 500-bed urban hospital was plagued by discharge delays, often waiting hours for ancillary services. By implementing an AI-driven capacity management system that integrated with their EHR, they created predictive discharge workflows. The system automatically notifies transport and housekeeping of likely discharges 4-6 hours in advance. Within a year, they reduced their average length of stay by nearly a full day, freeing up dozens of beds and significantly improving patient throughput.
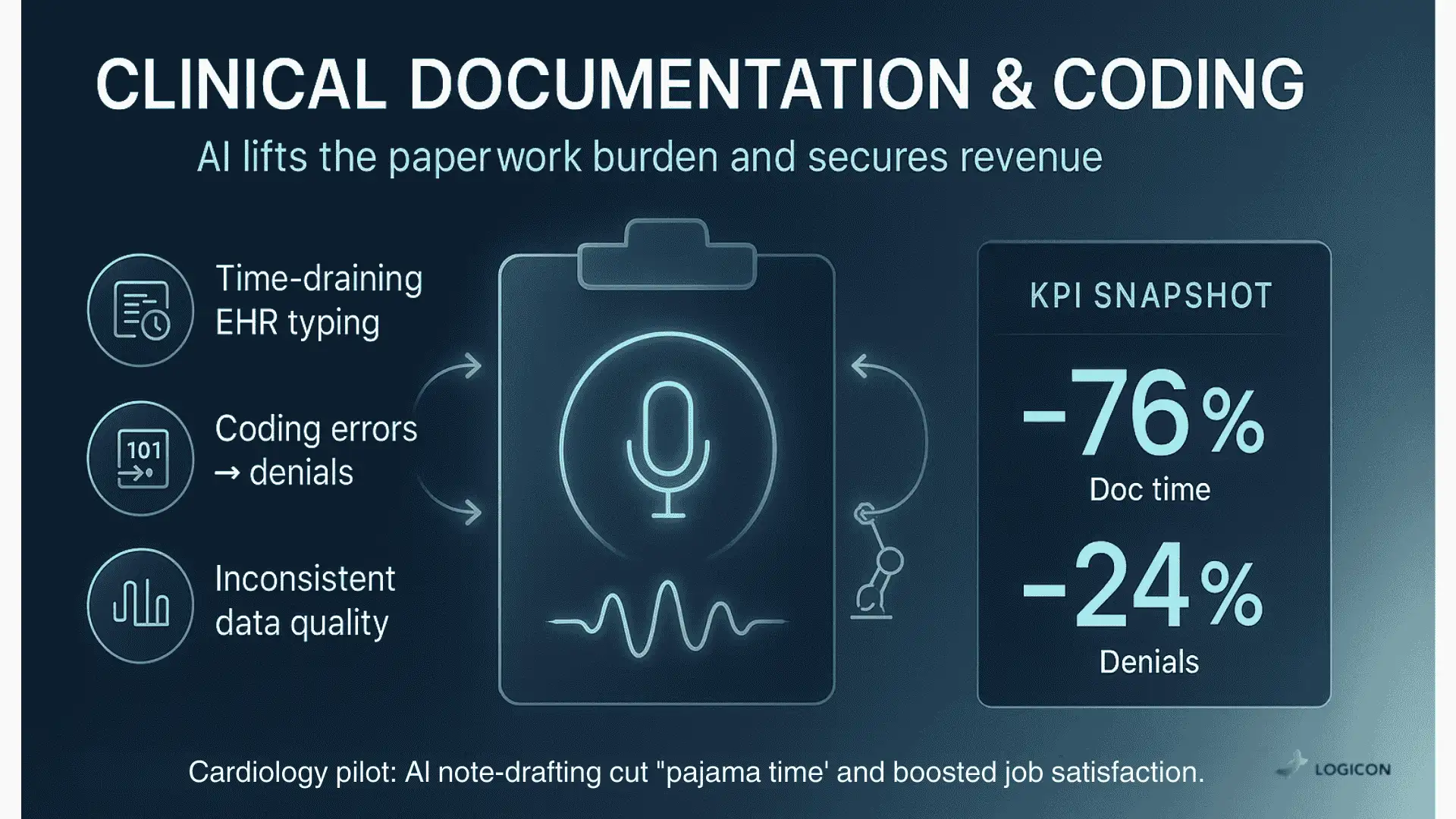
Workflow 2: Clinical Documentation & Coding
The administrative burden of clinical documentation is a primary driver of physician burnout. AI is now capable of lifting this burden, improving both the quality of work-life for clinicians and the accuracy of the data that drives the revenue cycle.
The Pain Points
- Clinicians spend excessive time on EHR data entry and note-taking.
- High rates of coding errors and omissions lead to claim denials.
- Inconsistent data quality that undermines analytics and quality reporting.
The AI Solution Set
- Ambient Clinical Voice: AI-powered microphones listen conversationally to the patient-provider interaction and automatically draft the clinical note in the EHR for the physician to review and sign.
- Computer-Assisted Coding (CAC): Natural Language Processing (NLP) scans the completed clinical note to suggest accurate medical codes (ICD-10, CPT), reducing human error and ensuring complete charge capture.
- Robotic Process Automation (RPA): Bots can handle the repetitive tasks of querying physicians for documentation clarification.
Implementation Essentials
Deep, secure integration with the EHR is non-negotiable. For the CIO, ensuring the AI models are HIPAA-compliant and that data is protected is paramount. For the operations director, a phased rollout with strong physician champions is key to overcoming initial skepticism and demonstrating value.
KPI & ROI Snapshot
- Primary Metrics: Physician documentation time, claim denial rate, coding accuracy, case mix index (CMI).
- Average ROI: Implementations have shown a reduction in documentation time by as much as 76% and a 24% decrease in coding-related denials.
Mini-Case Vignette
An academic medical center’s cardiology department was losing physicians due to burnout from after-hours charting. They piloted an ambient voice solution for their outpatient clinic. The AI’s ability to draft accurate, structured notes in real-time was a game-changer. The pilot group reported a dramatic drop in their “pajama time” spent on the EHR and a significant increase in job satisfaction, all while improving the detail and timeliness of their clinical notes.
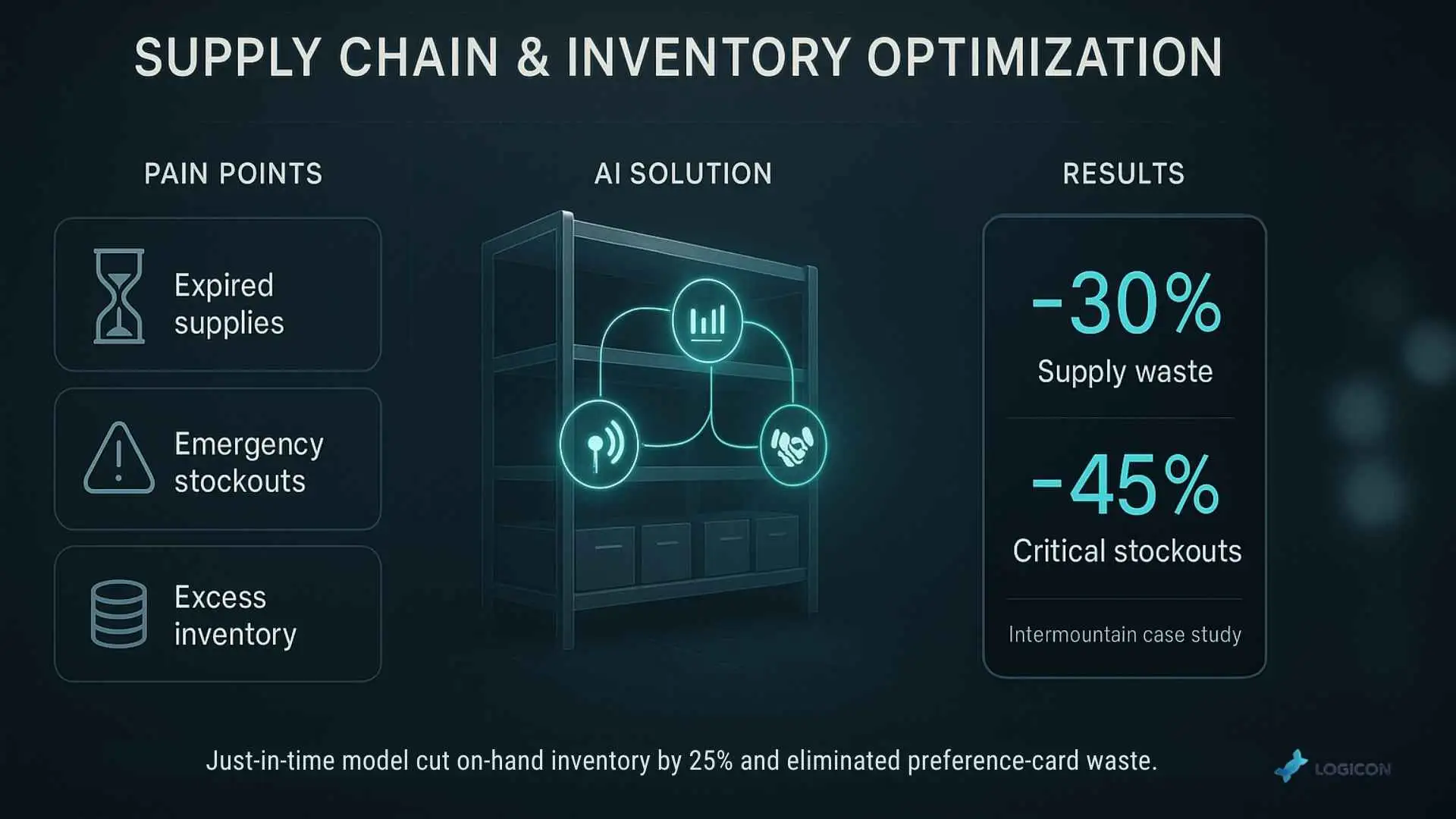
Workflow 3: Supply Chain & Inventory Optimization
In a low-margin environment, every wasted supply dollar counts. Traditional supply chains are often reactive, leading to both costly overstocking and dangerous stockouts of critical items. AI brings predictive power to inventory management.
The Pain Points
- High percentage of expired or wasted medical supplies.
- Unexpected stockouts of essential items are forcing expensive emergency orders.
- Massive amounts of capital are tied up in excess inventory.
The AI Solution Set
- Predictive Demand Forecasting: AI analyzes historical usage patterns, surgical schedules, and even seasonality to predict future supply needs with far greater accuracy than human forecasts.
- Automated Inventory Tracking: Using RFID tags or computer vision, AI can maintain a real-time count of supplies in store rooms and on carts, automatically triggering reorders when levels fall below a dynamic par level.
- Supplier Management: AI can analyze supplier performance data to identify risks and recommend optimal sourcing strategies.
Implementation Essentials
This requires tight integration between the AI platform, the hospital’s Enterprise Resource Planning (ERP) system, and the EHR. A successful project starts with a focused pilot, such as optimizing supplies for a single high-volume area like the orthopedic ORs.
KPI & ROI Snapshot
- Primary Metrics: Inventory carrying costs, supply waste percentage, stockout incidents, contract compliance.
- Average ROI: Health systems like Intermountain have used AI to cut supply waste by 30% and have seen stockouts of critical items fall by over 45%.
Mini-Case Vignette
A regional health network struggled with managing supplies for its various surgical departments. They deployed an AI-powered supply chain platform that integrated with their surgical scheduling system. By analyzing the specific preference cards of surgeons and the scheduled case volume, the platform created highly accurate demand forecasts. This allowed them to move to a just-in-time inventory model, reducing on-hand inventory by 25% and virtually eliminating preference-card-related waste.
Workflow 4: Smart Staff Scheduling & Workforce Analytics
Staffing is a hospital’s largest expense and its most valuable asset. Yet, scheduling is often a manual, painful process that leads to inequity, burnout, and costly overstaffing or understaffing. AI creates smarter, fairer, and more cost-effective schedules.
The Pain Points
- Heavy reliance on expensive overtime and agency nurses.
- There are high rates of staff turnover due to burnout and perceived scheduling inequity.
- There are mismatches between unit staffing and actual patient census and acuity.
The AI Solution Set
- Predictive Scheduling: AI models forecast patient demand on a unit-by-unit basis, allowing schedulers to build rosters that match the anticipated workload, not just a static grid.
- Automated Shift Filling: When a last-minute call-out occurs, AI can automatically text or message qualified and available staff members based on pre-set rules (e.g., avoiding overtime, offering bonuses), filling the shift in minutes instead of hours.
- Fairness Algorithms: The system can ensure equitable distribution of holidays and weekend shifts, a major driver of staff morale.
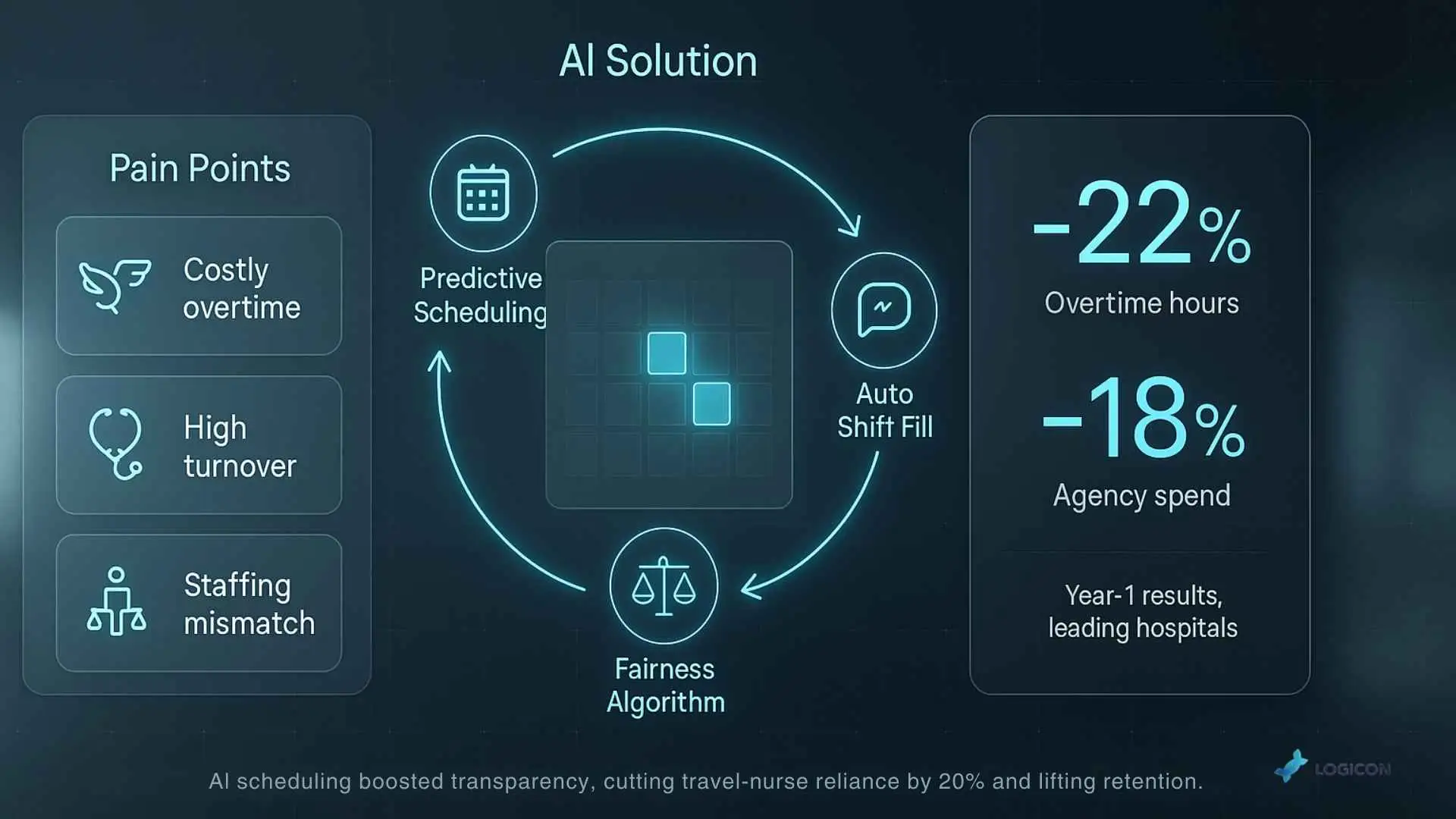
Implementation Essentials
This automation must integrate with the existing HR and timekeeping systems to function. Change management is vital to reassure staff that the goal is not to replace schedulers, but to give them more powerful tools to create a better work environment.
KPI & ROI Snapshot
- Primary Metrics: Overtime hours as a percentage of total hours, premium labor (agency) spend, staff turnover rate, time-to-fill open shifts.
- Average ROI: Leading hospitals have used these tools to reduce overtime by 22% and cut agency spend by 18% in the first year.
Mini-Case Vignette:
A large community hospital was battling a high nursing turnover rate, with exit interviews frequently citing unfair schedules. They implemented an AI scheduling platform that used predictive analytics to align staffing with patient load and automated the open-shift marketplace. The transparency and equity of the new system were an immediate hit. Within 18 months, the hospital reduced its reliance on travel nurses by nearly 20% and saw a measurable improvement in nurse retention rates.
Workflow 5: Revenue Cycle Acceleration
The path from patient care to payment is littered with manual tasks, administrative friction, and costly errors. AI automation streamlines this entire process, ensuring health systems are paid more quickly and entirely for the care they deliver.
The Pain Points
- There are high claim denial rates from payers due to administrative errors.
- Long Accounts Receivable (A/R) cycles, tying up critical cash flow.
- Enormous staff time is spent on manual prior authorizations and claim follow-up.
The AI Solution Set
- AI-Powered Prior Authorization: NLP and RPA bots can automatically assemble the required clinical documentation from the EHR and submit prior authorizations electronically, tracking them to completion without human intervention.
- Denial Prediction & Prevention: AI analyzes historical claim data to flag claims with a high probability of being denied before they are submitted, allowing staff to correct them proactively.
- Automated Claim Statusing: RPA bots can log into dozens of different payer portals simultaneously to check the status of outstanding claims, automating a task that consumes thousands of hours for billing staff.
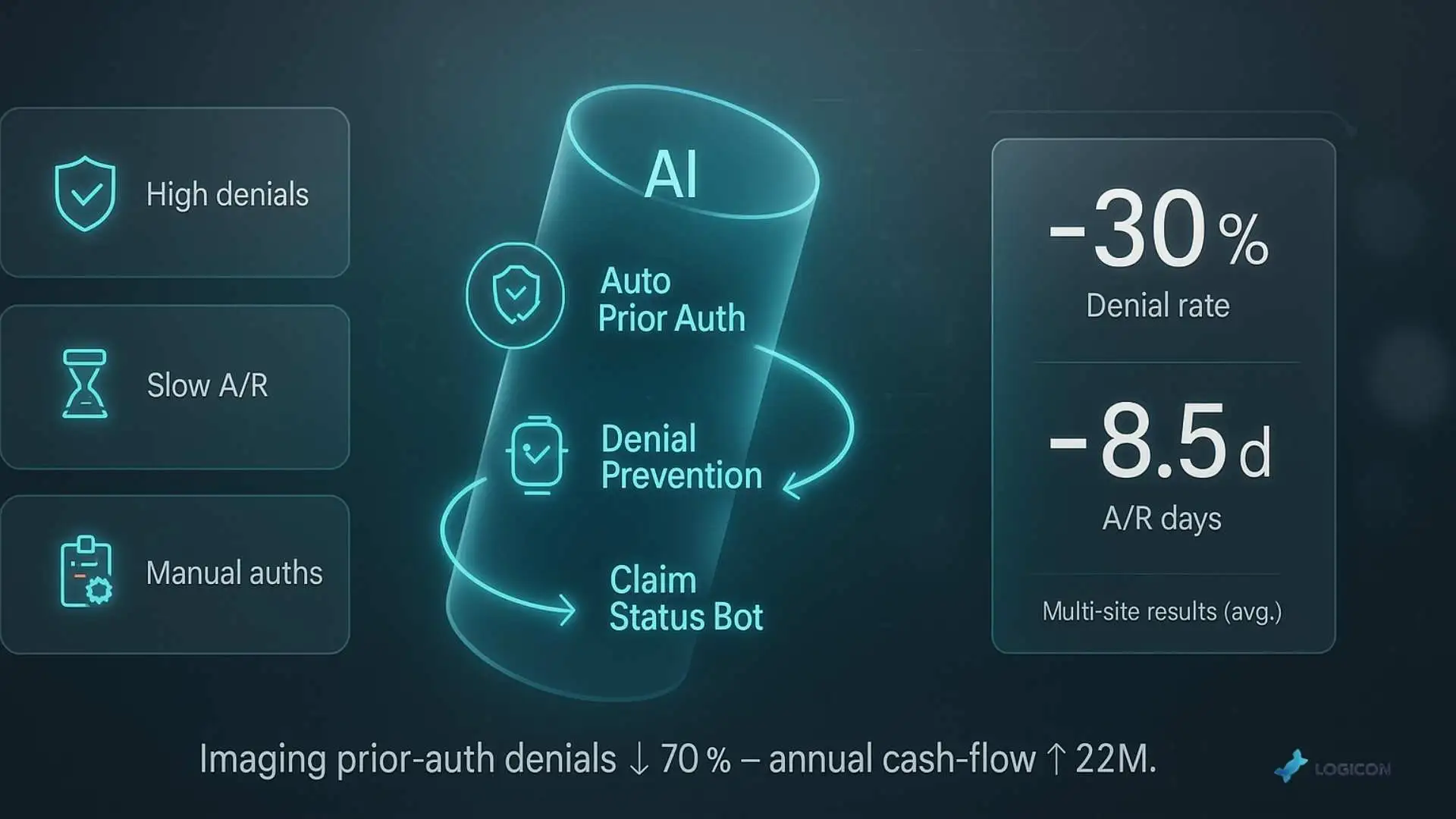
Implementation Essentials
This is where a robust, enterprise-grade integration strategy is most critical. A partner like Logicon can build the secure, resilient connections between the EHR, the billing system, and hundreds of payer portals, which is the technical backbone of revenue cycle automation.
KPI & ROI Snapshot
- Primary Metrics: First-pass denial rate, A/R days, cost to collect, prior authorization approval rate.
- Average ROI: Health systems have successfully lowered their denial rates by over 30% and reduced A/R days by an average of 8.5 days.
Mini-Case Vignette
A mid-sized health system’s billing office was overwhelmed by denials for high-cost imaging procedures. They implemented an AI platform to automate the prior authorization process. The system pulled clinical data directly from the EHR, submitted the request to the payer, and followed up automatically. This single intervention reduced prior authorization-related denials for imaging by 70% and accelerated cash flow by an estimated $2 million annually.
Implementation Playbook: A Roadmap for Success
Deploying AI is a journey, not a single event. A phased, strategic approach dramatically increases the odds of success.
- Readiness Assessment: Evaluate your data infrastructure, technical capabilities, and organizational culture.
- Data Governance & Integration Audit: Identify and map the core systems (EHR, ERP, Billing) that will fuel the AI. Ensure data is clean, standardized, and accessible.
- Pilot a Quick Win: Choose one high-pain, high-impact workflow for an initial pilot. Use a Prioritization Matrix to plot potential projects based on their operational impact versus their technical complexity. A project in the “High Impact, Low Complexity” quadrant, like automating claims status checks, is an ideal starting point.
- Build the Integration Backbone: Work with an enterprise integration partner to build the secure, scalable APIs and data pipelines needed for the pilot and for future scale.
- Scale & Optimize: Use the success of the pilot to build momentum and a business case for expansion. Scale the solution to other departments or begin a new pilot in a different workflow.
- Establish Continuous Governance: Create a cross-functional AI governance committee, including clinical, operational, IT, and compliance leaders, to oversee the program, monitor performance, and manage risk.
Avoiding Common Pitfalls
Many AI projects fail not because of the technology, but because of a failure to plan for everyday challenges.
| Failure Factor | Mitigation Tactic |
| Data Silos | Implement a robust, enterprise-wide data integration strategy before starting. |
| “Black Box” AI | Choose partners who provide explainable AI (XAI) so you can understand why a model makes a specific recommendation. |
| Poor User Adoption | Involve frontline clinicians and staff in the design and testing process from day one. Focus on solving their real-world problems. |
| Ignoring Security | Make cybersecurity and HIPAA compliance a core requirement from the outset, not an afterthought. |
| Unrealistic Expectations | Start with a focused pilot project to demonstrate value and secure buy-in before attempting a massive, system-wide overhaul. |
Building the Business Case for Automation
The financial argument for AI in operations is compelling. The average ROI for successful projects is 4.3 times the initial investment. A simple breakeven calculation can frame the business case for your board:
Breakeven Point (in months) = Total Implementation Cost / (Monthly Hard Cost Savings + Monthly Revenue Gains)
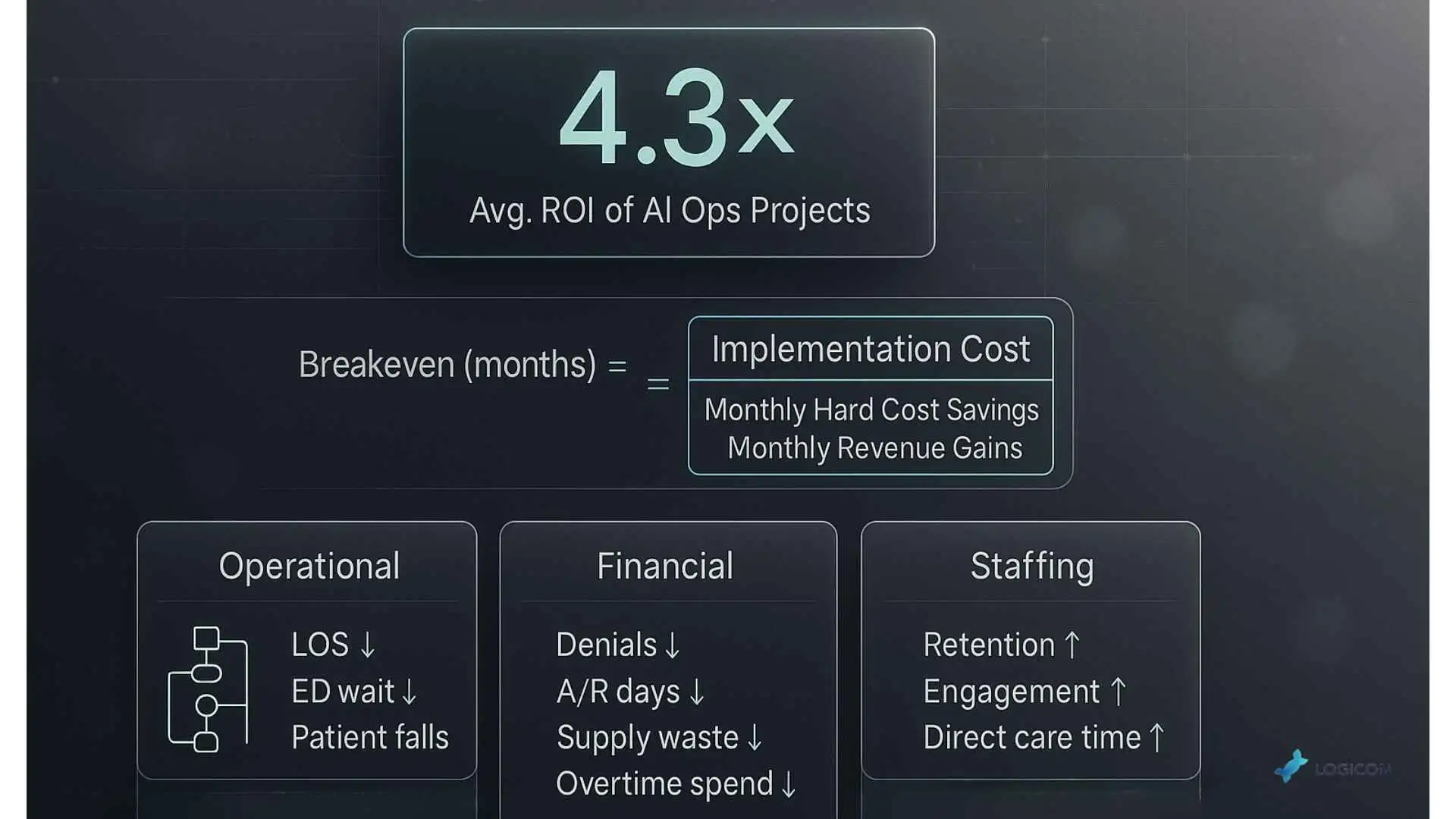
When presenting to leadership, focus on a balanced scorecard of metrics:
- Operational Metrics: Reduction in LOS, ED wait times, and patient falls.
- Financial Metrics: Reduction in denial rate, A/R days, supply waste, and overtime/agency spend.
- Staffing Metrics: Improvement in staff retention, engagement scores, and time spent on patient care.
Distinguish between hard cost savings (e.g., reduced agency labor, lower supply costs) and soft cost savings (e.g., avoiding burnout-related turnover, which has its own significant replacement cost).
The Future-Forward Edge: Staying Ahead of the Curve
The field of AI is advancing rapidly. A forward-thinking strategy prepares your organization for what’s next.
- Multimodal AI: Future systems will analyze not just text and numbers, but also medical images, audio, and even video to provide richer insights.
- Digital Twins: Hospitals will create virtual models of their operations to simulate the impact of changes—like a new staffing model or a new unit opening—before implementing them in the real world.
- Federated Learning: This approach allows AI models to be trained across multiple hospitals without the sensitive patient data ever leaving your firewall, improving model accuracy while preserving privacy.
Three Recommendations to Stay Ahead:
- Build for Data Fluidity: Your ability to participate in future innovations depends on having a modern, API-first integration architecture today.
- Monitor the Regulatory Landscape: Keep a close watch on evolving guidance from the FDA on AI as a Medical Device and from the ONC on algorithmic transparency.
- Prioritize Governance: A strong, ethical governance framework is the best way to ensure your use of AI is responsible, equitable, and future-proof.
Conclusion: Your Partner for Intelligent Automation
Intelligent automation is the key to unlocking a new level of operational efficiency in healthcare. It empowers staff by removing administrative friction, optimizes the use of scarce resources, and builds a more financially resilient organization. By focusing on high-impact workflows, health systems can begin a pragmatic journey that delivers immediate value and builds a foundation for future transformation.
The key to unlocking this potential lies in connecting these powerful AI tools to your core systems securely and reliably.
Ready to identify the highest-impact automation opportunities in your hospital? Schedule a complimentary 30-minute AI workflow assessment with Logicon.tech specialist today.