Subscribe to our newsletter
Every tick of the wall clock is a clinical decision deferred–or delivered. This article demonstrates how seven concrete technologies are providing bedside nurses with a precious half-hour (or more) every shift: less scrolling, less scavenging, and more human care.
Abstract
Hospitals that adopt automated medication cabinets, smart pumps, friction-free documentation, AI scheduling, continuous monitoring, voice assistants, and back-office bots are winning back an average of 34–47 nurse minutes per 12-hour shift. The reclaimed time translates to calmer units, lower overtime, shorter LOS, and—most importantly—safer patients. This article unpacks each win, shares frontline voices, and ends with a 90-day roadmap you can swipe today.
3:17 a.m., South Tower, Room 514
Tamika M., charge nurse, stifles a yawn and scans her dashboard.
Two overdue dressing changes. One rising creatinine. And four unanswered “Can I get ice chips?” lights blinking down the corridor.
Five years ago, Tamika would have jogged back and forth all night, clipboard in hand. Tonight, her innovative pump dashboard had already re-titrated a more accurate drip; the unit’s voice assistant logged Mrs. Lee’s vitals hands-free, and the automated cabinet delivered a stat Zosyn dose without a single phone call to the pharmacy. Tamika pours coffee, not sweat.
Automation did that.
Why Minutes Matter More Than Money
A single RN turnover costs roughly $56,300. Yet, most nurses don’t leave for pay–they leave because they can no longer do the work they were trained for. Administrative load eats 25%–41% of a shift. Give back just half an hour, and you create space for:
- A focused neurological exam that prevents a fall,
- A five-minute teach-back that averts a 30-day readmission,
- Or two quiet breaths that fend off burnout.
Below are the seven automations already tipping the scales.
1. Automated Medication Dispensing Cabinets
Time returned: 24–32 min/shift.
Before: Serpentine walks to the central pharmacy, manually counts narcotics, and uses sticky-note overrides.
After: Profile-based access steps from the bedside.
“Since the cabinets went live, I finish med pass before breakfast trays roll in–and my patients notice.”
—Jackson A., RN, Med-Surg
What works:
- Single-sign-on badges shave 6 clicks per withdrawal.
- Real-time inventory sync slashes “missing med” pages by 83%.
ROI snapshot: One Midwest system cut monthly medication waste 24%, saving $4.1M in year one.
Quick-start tip: Map the last 10 feet of the workflow; if a cabinet sits behind a linen cart, you just re-created a bottleneck.
2. Smart Infusion Pumps with EHR Interoperability
Time returned: 15–25 min/shift.
Keypad programming once meant 30 button presses–and three double-checks. Auto-programming now drops that to four. Autodoc writes the MAR line item as soon as the line starts.
Safety dividend: 77% cut in wrong-rate errors at a 316-bed community hospital.
| Metric | Pre-interoperability | Post | Delta |
| Avg programming time | 8.4 min | 1.9 min | −77% |
| Keystrokes | 120 | 17 | −86% |
Implementation pearl: Build the drug library with frontline nurses; they’ll spot the missing heparin concentration before go-live saves you.
3. Friction-Free Documentation & Device Integration
Time required: 30–45 minutes per shift.
Sly truth: nurses don’t hate EHRs–they hate redundancy. When vitals, pump rates, and bed-exit alarms are set to flow automatically, note that time plummets.
Case in point: a 42-bed step-down unit in Virginia reclaimed 64,800 nursing hours annually after wiring monitors to the chart and pruning 17 “just-in-case” flowsheet rows.
“I document in real-time, not recall. That means my chart tells the truth, not my best guess at 10 p.m.”
—Elena R., RN-BC
Design cue: Hide raw device data behind hover layers; show trends upfront. Clinicians want answers, not numbers.
4. AI-Powered Scheduling
Time returned (manager): 5 h / month
Indirect nurse minutes: 8–12 min/shift
An AI scheduler ingests acuity forecasts, PTO requests, and union rules, then spits out a balanced grid in 90 seconds.
- 37% drop in last-minute agency calls
- 9.8 pt rise in “schedule fairness” on engagement survey
Why Omar cares: Smoother staffing directly correlates with lower LOS and higher HCAHPS scores. Balanced assignments reduce call-outs, which in turn lead to fewer overtime hours.
Adoption hack: Let staff game the algorithm during rollout–two cycles of sandbox play to build trust before the roster is real.
5. Continuous Remote Patient Monitoring
Time required: 20–30 minutes per shift.
Wearable sensors stream vital signs to a central console; nurses stride to beds only when the trend line indicates trouble.
Clinical punch: Early sepsis alerts climbed from 54% to 88%. Step-down transfers fell 14%.
“The beeping IV had my attention; the silent tachycardia on the dashboard saved the patient.”
—Derrick K., RN
Alarm fatigue fix: Tie alerts to a three-strike logic (rate, duration, trend) so phones buzz for a signal–not noise.
6. Voice Assistant Workflows
Time returned: 15–22 min/shift
At the bedside:
“Hey Clara, add 2 mg morphine IV now.”
Order lands in the EHR; the pharmacist eyes it instantly.
During rounds:
“Show me potassium last 6 hours.”
The result flashes on the Ascom handset–no mouse, no alt-tab.
Early pilots log 3.3 hours/week of documentation relief per clinician.
Cultural note: Provide a “quiet room” for staff to practice commands. Laughter is good change-management fuel.
7. Back-Office Robotic Process Automation (RPA)
Indirect time returned to floor: 5–10 min/shift
Bots registering patients, posting remits, or compiling discharge packets spare clerks hours, which shrinks the “Where are my papers?” interruptions nurses dread.
- One Dublin hospital reclaimed 3 hours a day by automating ICD code entry.
- A US payer-mix site cut claim cycle time 50%, accelerating bed turnover.
Scale rule: Start with a single sub-process (e.g., eligibility check). Success breeds bot budgets.
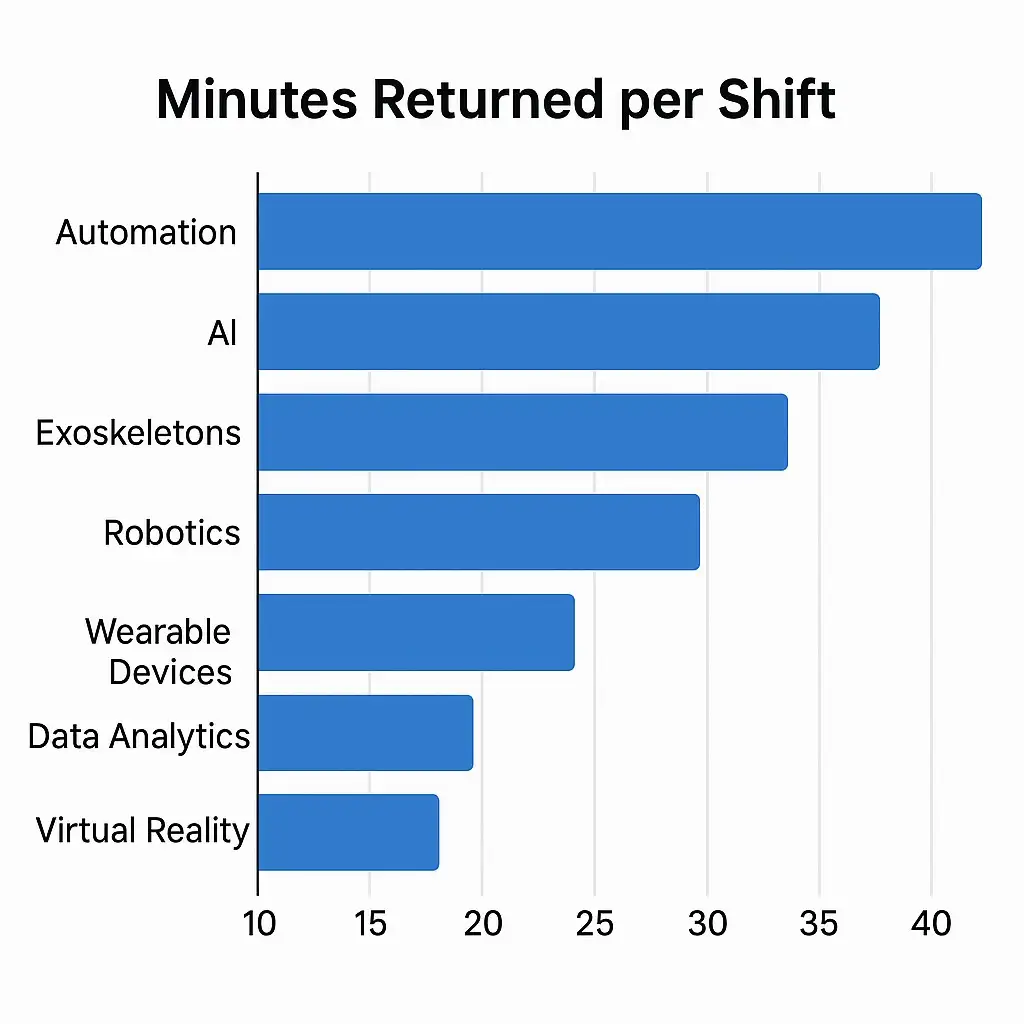
Synthesizing the Wins
Add the conservative ends of each range, and a 32-bed unit frees >110 nursing minutes each shift–nearly one FTE. This surplus converts to:
- 0.4-day reduction in average LOS (when bedside education happens on time)
- 12% drop in nurse overtime
- 6-point jump in HCAHPS “nurse communication” domain
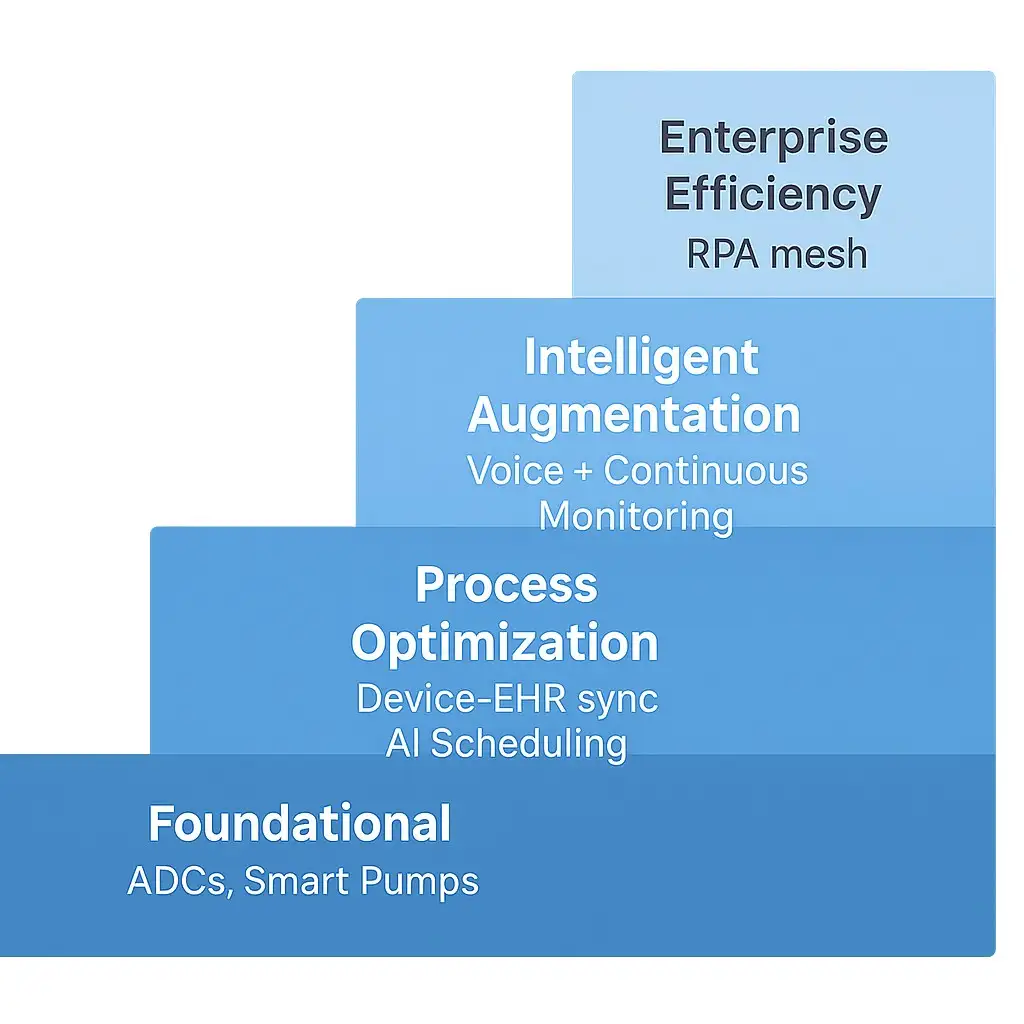
The Automation Adoption Ladder
Your 90-Day Roadmap to a First Win
| Day 0-30 | Day 31-60 | Day 61-90 |
| • Pick a champion unit (ideally Med-Surg).• Baseline KPIs: med pass time, nurse OT, LOS.• Form cross-functional squad (RN, pharm, IT, finance). | • Choose one low-complexity tech (voice or Scheduling).• Co-design workflow; run simulations.• Over-communicate intent: “Give back minutes, not replace people.” | • Go live with at-elbow support.• Huddle daily, tweak quickly.• Publish the win: minutes saved, smiles captured.• Plan scale or next-rung tech. |
Need a sherpa? Logicon’s Change Management team has piloted 40+ automations without a single “pilot graveyard” casualty. Let’s talk.
FAQs: Real-World Wins That Give Nurses 30 Minutes Back
Q1. Will automation erode nursing judgment?
No. The systems handle rote, repeatable clicks, not critical thinking. Nurses still validate every med, review every alert, and decide every intervention.
Q2. We run three legacy EHR modules. Can this still work?
Yes. Middleware APIs–or, as a bridge, RPA–let data flow without a forklift upgrade. Logicon specializes in hybrid environments.
Q3. What KPIs show success fastest?
Review the documented nurse time in the EHR audit log, overtime hours, and time-to-first-dose for new admissions. Improvements appear within weeks.
Q4. How do we fund the project?
Many hospitals earmark a portion of their agency-nurse spending. One client redirected two months of agency savings to finance a cabinet rollout–ROI was achieved in month seven.
Conclusion: Time Is Care
Tamika’s shift ends at 7:05 a.m. She hands off a stable roster, logs out, and slips a thank-you note from Mrs. Lee into her pocket. “You sat with me when I couldn’t sleep,” it reads.
Automation gave Tamika that minute. Multiply it by every nurse, every night, and you rewrite the rhythm of care.
Ready to see your numbers?
Book a 20-minute workflow discovery call with Logicon’s Nursing Informatics group. We’ll model your current time sinks and sketch the fastest path to your first 30-minute win.